Evolving role of the Interleukin-5 antagonist mepolizumab for hypereosinophilic syndrome: pathogenesis and advances in therapy - A narrative review
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
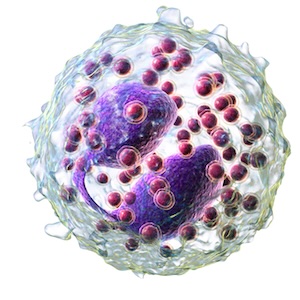
Hypereosinophilic syndrome (HES) is a rare blood disorder characterized by hypereosinophilia greater than 1,500/μL on at least two separate occasions with some degree of associated end-organ damage and exclusion of other identifiable causes of hypereosinophilia. The systemic effects and damage seen in HES can be extensive, resulting in a variety of clinical presentations, but most commonly the affected organs include the lungs, heart, skin, and the gastrointestinal tract. After FDA-approval in 2020, mepolizumab (trade name Nucala) an interleukin-5 (IL-5) antagonist monoclonal antibody, is considered an effective treatment for HES given its ability to lower absolute eosinophil counts, improve the symptomatic burden, reduce the number of HES flares experienced, and limit the need for corticosteroids as a primary therapy. Also of benefit, Nucala has been shown to have a positive safety profile with limited adverse effects and no notable contraindications to treatment.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






